Background
Approximately 6% of patients with sciatic nerve pain have piriformis syndrome Source. Sciatic nerve pain is often debilitating, leading to symptoms such as extreme pain, numbness, and weakness. After my experience dealing with piriformis syndrome long term I would define piriformis syndrome as an unmet medical need.] because there is not an extensive playbook that clinicians have to help their patients.
In piriformis syndrome, the piriformis muscle irritates the sciatic nerve leading to symptoms such as pain, numbness, and weakness down the leg.
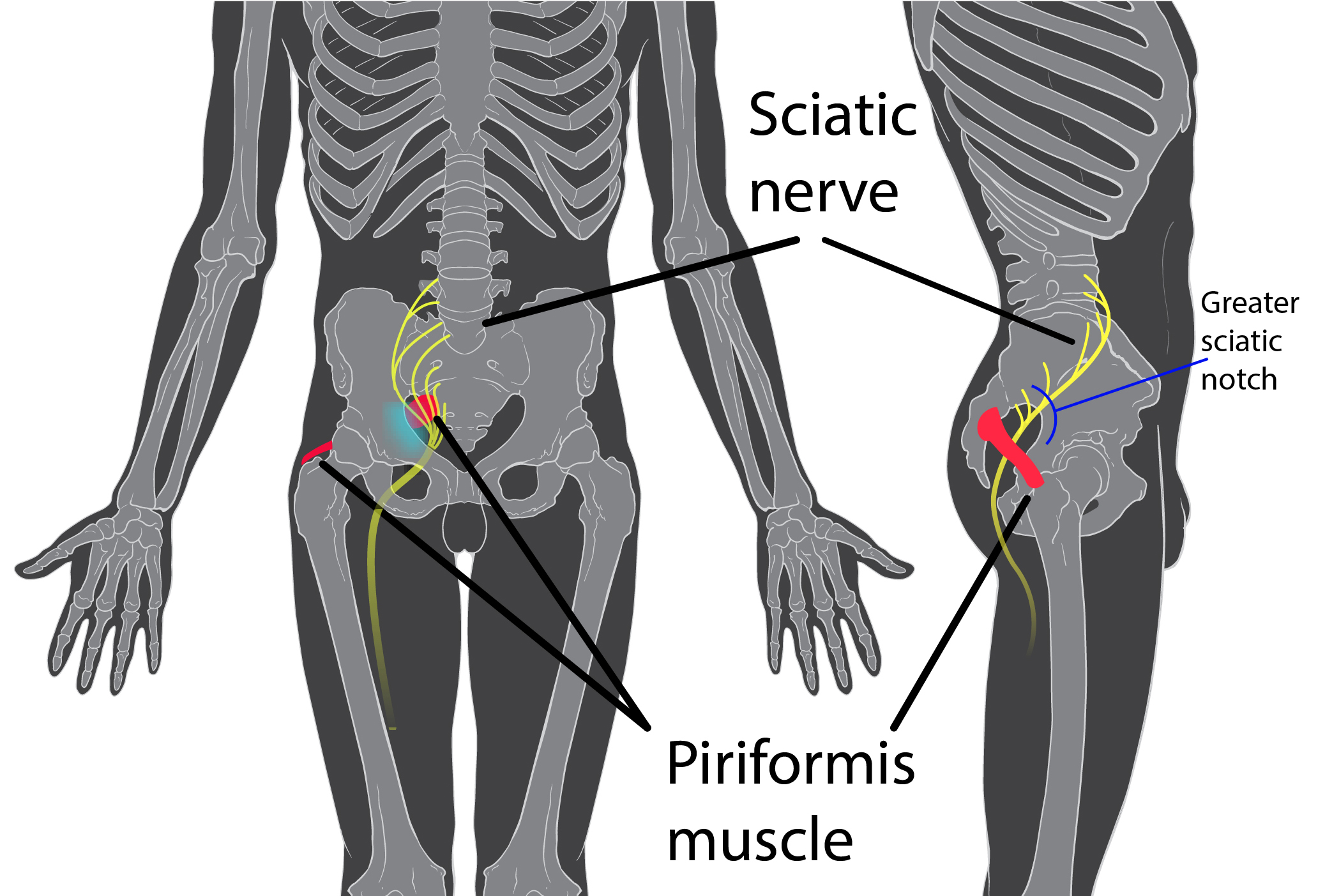
“In as much as 22% of the population, the sciatic nerve pierces the piriformis muscle, splits the piriformis muscle, or both, predisposing these individuals to piriformis syndrome. The sciatic nerve may pass completely through the muscle belly, or the nerve may split—with one branch (usually the fibular portion) piercing the muscle and the other branch (usually the tibial portion) running inferiorly or superiorly along the muscle” Source. The best practice treatments are stretching, physical therapy, and steroid injection. Steroid injection has long been treated as a conservative treatment option, but recent evidence from Boston University as shown otherwise. While these can resolve most cases, there are many cases that do not clear and impact the quality of life of the patients living with the syndrome. Surgery is considered a last resort for piriformis syndrome, and has a poorer significantly longer recovery than other common sciatic pain relief surgeries such as microdiscectomy. This is because the tissue surrounding the piriformis is typically cut away, leading to a recovery time of 3-4 months even when done endoscopically.
Alternative treatments?
Approximately 80% of cases clear up with conservative treatment Source. Where does that leave the rest of us? If pain is your issue some find relief with TENS, but clinical evidence for TENS is not particularly strong. For patients like myself with numbness and weakness rather than pain there is not a treatment method with a good risk profile. From the above rates of occurrence, approximately 1% of patients presenting with sciatic nerve pain have piriformis syndrome that does not resolve with conservative treatment (6% of sciatic nerve pain multiplied by 20% of cases not resolving with conservative treatment).
Prevalence
It is difficult to estimate the number of piriformis syndrome cases annually as the reporting and diagnosis is not effective, but I will give it my best shot. Sciatic nerve irritation accounts for ~5-10% of low back pain annually Source. Of that, 6% is likely piriformis syndrome (0.3%-0.6%). Prevalence estimates of low back pain in the U.S. range from 1.4%-15.6% Literature Review of Low Back Pain. This indicates a range of 0.004%-0.094% prevalence of piriformis syndrome. This puts the range estimate for patients at ~13,000-300,000 people living with piriformis syndrome, with at 3,000-60,000 having cases that will not clear up with conservative treatment.
Does this represent a market opportunity?
The market is too small for a device that requires a PMA from the FDA unless the price is very high. Currently, some pharmacological treatments exist but they are not targeted specifically at piriformis. The density of patients needing more than conservative treatment is very low even with the high end estimate of 60,000 people living with pain. Diagnosis is difficult because the symptoms are commonly shared with bulging/herniated discs, meaning many patients that could benefit would not even have the chance to know what is ailing them. These barriers likely mean that there will not be a device or treatment that specifically targets piriformis syndrome coming to the market and any general nervous system/muscle spasm treatment will think of the piriformis as a distant afterthought. Until the incentives shift enough to bring about new treatment modalities, massage therapy and stretching will remain the best way to tend to this pain in the butt.
